Presentation
- Resuspended Red Cells - 220-340mL
- Paediatric Packs - each donation is divided into 4 paediatric doses - 55-85mL
- Haematocrit-adjusted blood is used for neonatal exchange transfusions and intrauterine transfusion
- Whole Blood - 405-513mL
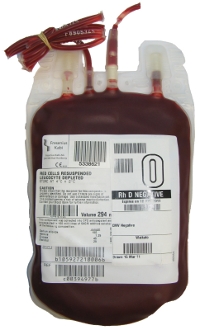
ABO & RhD Compatibility
ABO
- a group O patient can receive only group O red cells
- a group A patient can receive group A or O red cells
- a group B patient can receive group B or O red cells
- a group AB patient can receive group AB, A, B or O red cells
- ABO incompatible transfusions can be fatal. Always check the the red cells against the patient at the bedside.
Rh(D)
- Transfusion of red cells are normally Rh(D) identical
- Rh(D) negative red cells may be given to Rh(D) positive recipients without creating any risk for immunisation
- In life threatening emergencies, Rh(D) positive cells may be given to an Rh(D) negative recipient but there is a risk that this will stimulate the production of anti-D. The Blood Bank will provide guidance. The Clinician must be notified.
- Rh(D) positive red cells may be provided by the Blood Bank for males, and for females beyond reproductive years, if supplies of Rh(D) negative red cells are low.
Storage
- Must be stored in an appropriately monitored (2-6°C) blood refrigerator according to Blood Bank standards. Never store in a drug or food fridge.
- If the transfusion can not be started within 30 minutes, return the component to the Blood Bank immediately for appropriate storage.
Filter
- Use a standard blood infusion set that has a 170-200 micron filter.
- The infusion set should be changed when the transfusion is complete, or after 12 hours.
- All fresh components, including FFP and cryoprecipitate, are leucodepleted at source by NZBS. No bedside leucodepletion is necessary.
Pump
- If necessary, approved infusion pump devices may be used.
Rate and Duration
- Paediatrics:
- top-up transfusion in a non-bleeding patient is typically given at 5mL/kg/hr
- exchange transfusion: depends on stability of the baby - discuss with NICU consultant
- resuscitation: rapid infusion based on the patient's haemodynamics
- Adults:
- top-up transfusion in a non-bleeding patient: most adults will tolerate one unit every 90 minutes. Consider a slower rate in patients with or at risk of congestive cardiac failure
- resuscitation: rapid infusion based on the patient's haemodynamics
- Infusion of all components should be completed within 4 hours of leaving refrigerated storage.
Monitoring
- See page on Observations
DO NOT
- DO NOT add medication to red cell components
- DO NOT use 5% Dextrose solutions (may induce haemolysis)
- DO NOT use Lactated Ringer's or other balanced salt solutions that contain Calcium, as this may induce clot formation in the blood bag and / or administration set.
Dose
- 4-5mL/kg will raise the patient's Haemoglobin level by approximately 10g/L.
- It is recommended that the patient's haemoglobin be checked between units if giving multiple units.
- For paediatric patients, the dose should be written in mL, not units.
Dose calculator
More Info
- Patient Information Leaflet
- Datasheets
- Transfusion Medicine Handbook
- ANZSBT Guidelines on how to administer blood products
- TACO Pre-Transfusion Risk Assessment Tool
- NZBS policy on the provision of CMV antibody negative blood components
- NZBS policy on the use of fresh blood
- NZBS Clinical Compendium
- Patient Blood Management guidelines