How to administer Fresh Frozen Plasma or Thawed Plasma (FFP or FFP-EL) - Quick Guide
|
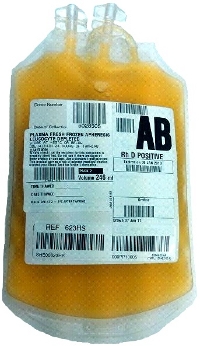
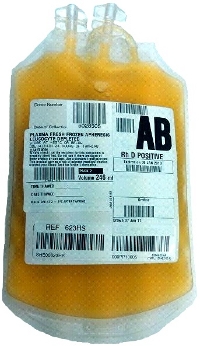
Presentation
|
- Fresh Frozen Plasma or Thawed Plasma (FFP or FFP-EL): 180-340mL
- Paediatric FFP: 45-90mL (4 doses can be obtained from a single donation)
- Please note that some blood banks in New Zealand are using FFP (24 hour shelflife) and some are using FFP-EL (120 hour shelflife).
Blood banks using FFP-EL are: Auckland, Christchurch, Dunedin, MidCentral, Middlemore, Tauranga, Waikato, Wellington.
|
|
|
ABO & RhD Compatibility
|
ABO
- Plasma components should be ABO compatible as follows:
- a group O patient can receive FFP or FFP-EL of any ABO group
- a group A patient can receive A or AB FFP or FFP-EL
- a group B patient can receive B or AB FFP or FFP-EL
- a group AB patient can receive only AB FFP or FFP-EL
- an unknown group patient can receive only AB or low titre group A FFP or FFP-EL
- Emergency FFP or FFP-EL is supplied as AB or low-titre A
Rh(D)
- No anti-D immunoglobulin need be given if Rh(D) negative patients receive Rh(D) positive FFP or FFP-EL or cryoprecipitate.
- Although frozen plasma components may contain small amounts of red cell stroma, sensitisation following transfusion of Rh(D) positive units is most unlikely, as stroma is less immunogenic than intact red cells.
Therefore Cryoprecipitate of any Rh(D) type may be given regardless of the Rh(D) type of the recipient. Contact Blood Bank if you are not sure.
|
|
Storage
|
- FFP or FFP-EL (24 or 120), once thawed, must be stored in an appropriately monitored (2-6°C) blood refrigerator according to Blood Bank standards for up to 24 or 120 hours.
- Never store in a drug or food fridge.
- If the transfusion can not be started within 30 minutes, return the component to a blood refrigerator Bank immediately for appropriate storage.
- Blood Bank will only accept the unit back into stock if returned within 30 minutes of issue from Blood Bank.
- Once issued, Fresh Frozen Plasma or Thawed Plasma should be transfused as soon as possible.
|
|
Filter
|
- Use a standard blood infusion set which has a 170-200 micron
filter
- ANZSBT guidelines require that blood giving sets must be changed when transfusion is completed or every 12 hours if the transfusion episode is not yet complete. This is intended to reduce the risk of bacterial growth occurring.
- Any number of red cell units may be transfused during a 12-hour period provided the flow rate remains adequate. However specific manufacturer's recommendations defining the maximum number of units per blood administration set must not be exceeded.
- A new blood administration set should be used if infusion of another fluid, medication or platelets is to continue after the current transfusion. This is intended to reduce the risk of incompatible fluids or drugs causing haemolysis of residual red cells in the administration set or drip chamber.
- Please consult your DHB blood policy for further details.
- All fresh components, including Fresh Frozen Plasma or Thawed Plasma, are leucodepleted
at source by NZBS. No bedside leucodepletion is necessary.
|
|
Pump
|
- Approved infusion pump devices may be used.
|
|
Rate and Duration
|
- Paediatrics:
- in a non-bleeding patient: infuse at 10-20mL/kg/hr
- resuscitation: rapid infusion based on the patient's haemodynamics
- Adults:
- in a non-bleeding patient: most adults will tolerate one unit of FFP or FFP-EL every 90 minutes. Consider a slower rate in patients with or at risk of congestive cardiac failure.
- resuscitation: rapid infusion based on the patient's haemodynamics
- Infusion of all components should be completed within 4 hours of leaving refrigerated storage.
|
Monitoring | |
|
DO NOT
|
- DO NOT add medication to FFP or FFP-EL or Cryoprecipitate
- DO NOT use 5% Dextrose solutions (may induce haemolysis)
- DO NOT use Lactated Ringer's or other balanced salt solutions that contain Calcium, as this may
induce clot formation in the blood bag and / or administration set.
|
|
Dose
|
|
|
Dose Calculator
|
|
|
More Info
|
|